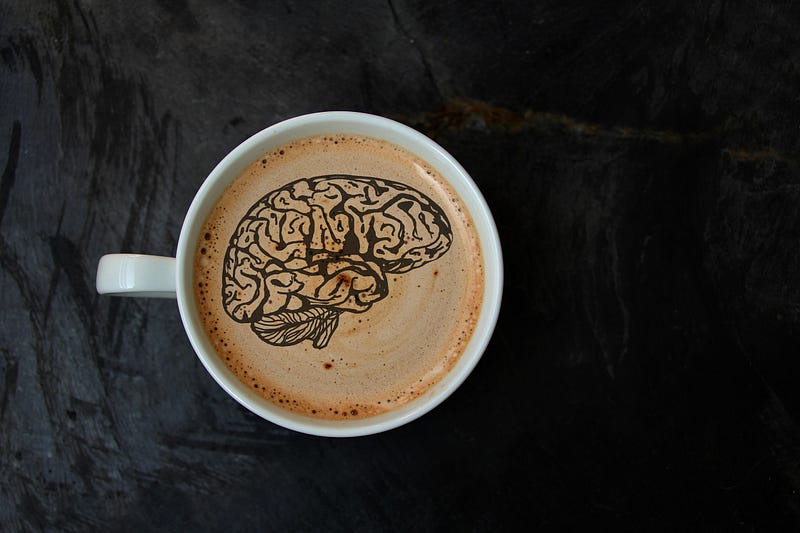
Every day, billions of people drink caffeine. Their reasons for this differ. Either they are relying on it to wake up, or to get through an afternoon slump, or maybe a night shift.
Caffeine is a well-known natural stimulant and is one of the most widely-used ingredients globally (1).
One of the main reasons caffeine is popular is its negative effects on the brain, including anxiety and sleep. But then, several studies have commended its many health benefits.
This article examines the effects of caffeine on your brain, as well as how it affects your sleep and your health in general.
 |
| How caffeine can affect your nervous system. |
What is Caffeine?
It is a natural stimulant widely found in coffee, cacao, and tea plants. It stimulates the central nervous system and the brain and helps you to remain alert while also preventing fatigue.
According to history, the very first tea was brewed in 2737 BC (1).
It was discovered by a shepherd in Ethiopia who observed that it gave his flock extra energy. And then, in the late 1800s, caffeinated soft drinks came on board, followed by energy drinks.
Currently, over 80% of the global population takes at least one caffeinated product each day. In North America, over 90% of adults take caffeinated products daily (1).
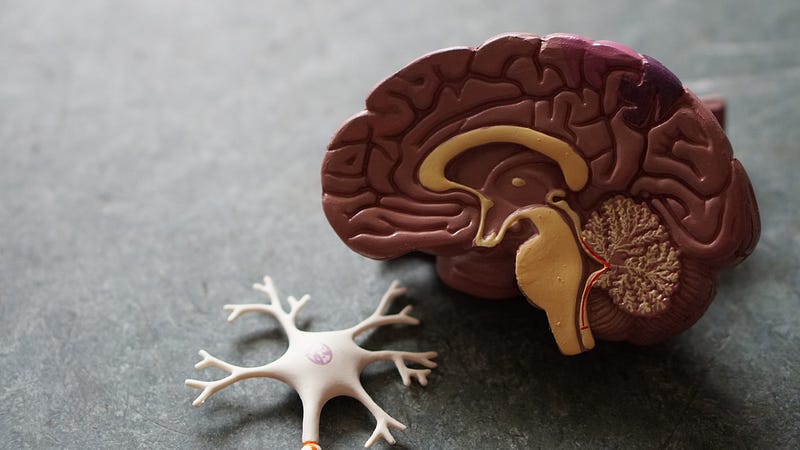
How Does Caffeine Affect Your Brain?
After caffeine is consumed, it is absorbed from the digestive system into the bloodstream. Once in the bloodstream, it moves to the liver and is metabolized (broken down) into elementary compounds that can affect your organs and how they function.
However, the main effect of caffeine occurs in the brain. Caffeine blocks adenosine’s effects. Adenosine is a neurotransmitter that causes your brain to relax and gives you that tired feeling (2).
Normally, the adenosine levels in your body build up over time, causing you to feel tired and give you that sleepy feeling.
But caffeine will keep you mentally alert and awake by binding to adenosine receptors but without activating them. This will block adenosine’s effects, thus reducing tiredness (3).
Caffeine also increases the level of adrenaline in the blood and the activities of norepinephrine and epinephrine in the brain (3).
This stimulates the brain and triggers a state of alertness, focus, and arousal. Caffeine is classified as a psychoactive drug because of its potential to affect your brain. Also, caffeine is “quick-acting.” For example, the amount of caffeine present in a cup of coffee can reach your bloodstream within 20 minutes, while its full effects can be felt within an hour of taking it (1).
Foods that Contain Caffeine
Caffeine is found naturally in nuts, leaves, or the seeds of certain plants. These sources are then harvested and processed, resulting in the production of caffeinated beverages and foods.
Below, we have the amounts of caffeine you may get per 240ml serving of some beverages (1):
- Coffee: 102–200mg
- Espresso: 240–720mg
- Energy drinks: 50–160mg
- Yerba mate: 65–130mg
- Chocolate milk: 2–7mg
- Cocoa beverage: 2–7mg
- Decaffeinated coffee: 3–12mg
- Soft drinks: 20–40mg
You can also find caffeine in some foods. For example, an ounce (28g) of milk chocolate contains 1–15mg, while an ounce of dark chocolate will provide 5–35mg (4).
Caffeine is also present in some over-the-counter drugs or prescription drugs like pain, allergy, and cold medications. It is also used in weight loss supplements.